Joint letter from the Chief Medical Officer Professor Anthony Lawler and Commissioner Liz Hefren-Webb to Board Chairs, Residential Aged Care Providers on winter preparedness in residential aged care.

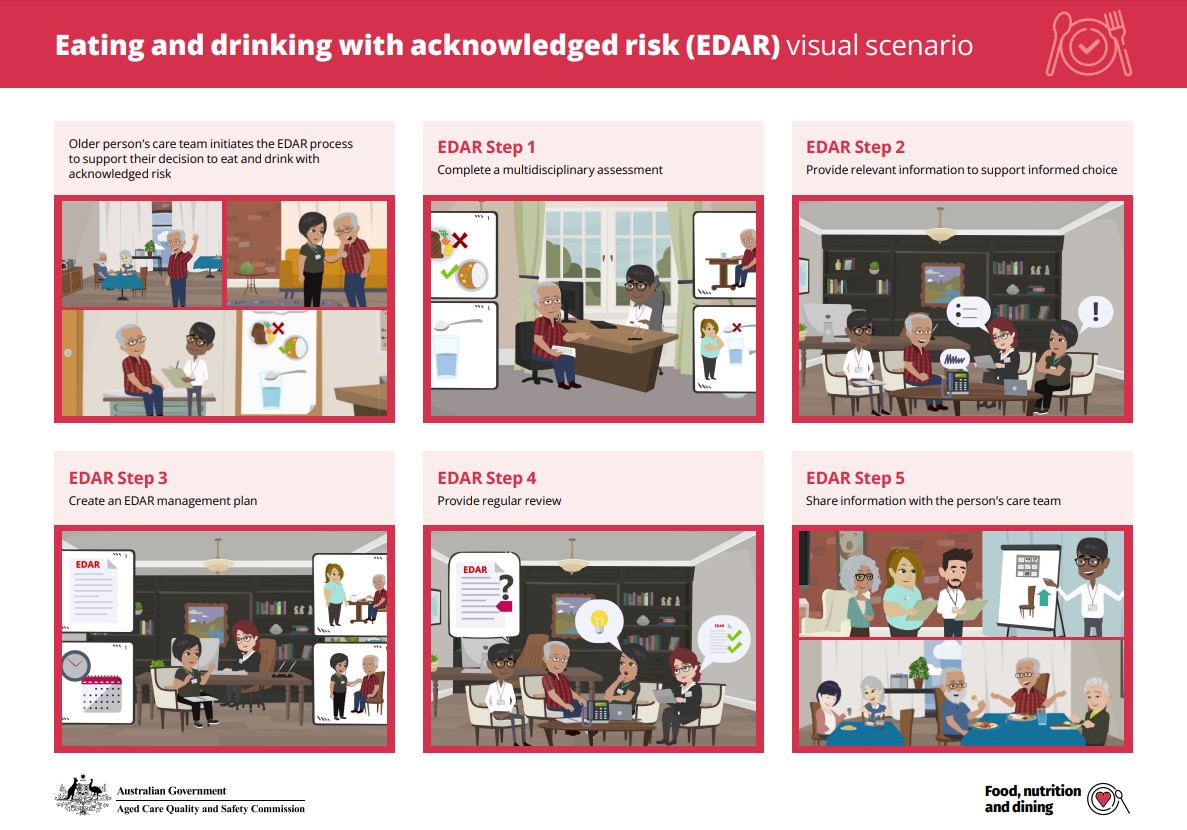
This visual scenario and supporting user guide has been designed to support aged care workers with information about eating and drinking with acknowledged risk (EDAR). It explains the best practice and practical strategies that providers should use when implementing EDAR in their service.
Outbreak management planning is a key part of infection prevention and control. This document supports both the development of a new outbreak management plan (OMP) and the quality assurance of existing plans. It details common OMP sections to get you started as you tailor your OMP to your service.
This resource may refer to information that will be updated from 1 July 2025 to align with the new Aged Care Act and Quality Standards.
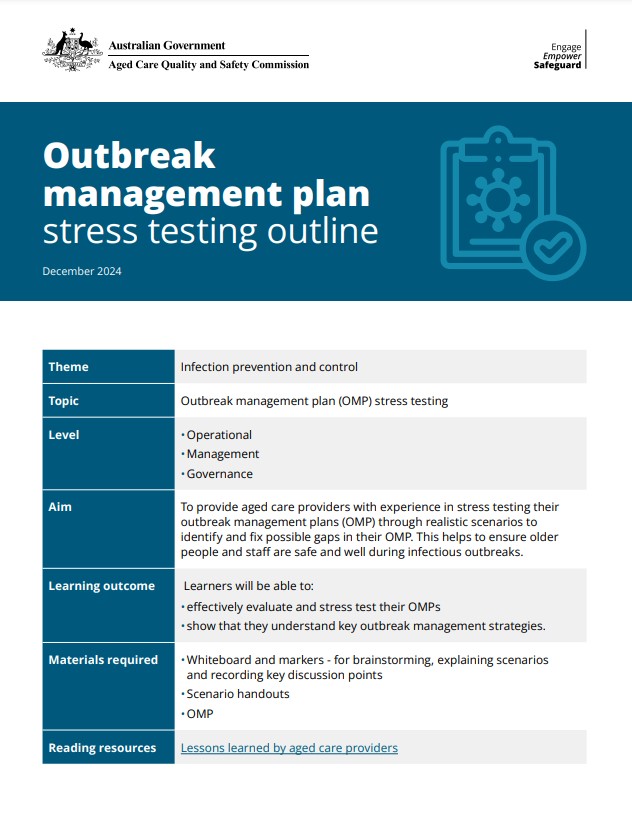
Having a comprehensive and organisation-specific outbreak management plan (OMP) helps your organisation to be prepared for the management of infections and outbreaks within your service. A key part of this readiness is ensuring that your OMP is fit-for-purpose and that everyone across the organisation can implement it if required. One way to maintain readiness and support continuous improvement of your OMP is to run regular drills, or stress tests, of your plan.
On Thursday 10 December 2020, the Aged Care Quality and Safety Commissioner Janet Anderson hosted a webinar on the recently released new outbreak management planning in aged care guide for aged care providers.

To support the aged care sector, the Commission has developed a range of storyboards that are designed to illustrate key behaviours and priority issues. The storyboards are particularly helpful in supporting people whose English or literacy levels may be a barrier when it comes to accessing content and are relevant to all providers and consumers, their families and representatives across the aged care sector.
Advance Care Planning – Don’t Leave it Too Late

This discussion paper explores strategies to improve medication management in aged care, including reducing inappropriate prescriptions and promoting non-pharmacological interventions. It reviews current interventions' effectiveness, highlights the use of psychotropic medications, and identifies areas for improving practices through multifaceted and multidisciplinary approaches for better resident outcomes and healthcare quality.
This resource may refer to information that will be updated from 1 July 2025 to align with the new Aged Care Act and Quality Standards.

On Thursday 6 August 2020, the Commission held a webinar for NSW/QLD-based providers of residential aged care services to share insights from the Commission’s work in monitoring and supporting services to prepare for and respond to an outbreak.

States and Territories have established directions giving effect to the Australian Health Protection Principal Committee’s recommendation that visitors and staff (including visiting workers) should not be permitted to enter a residential aged care facility, if they have not been vaccinated against influenza (after 1st May 2020).
Residential aged care facilities may wish to display the attached poster at entrances, to alert anyone entering the facility of these flu vaccination requirements.

Six steps for safe prescribing antipsychotics and benzodiazepines in residential aged care.
If you’re thinking of prescribing these medicines to manage the behaviours and psychological symptoms of dementia, follow these 6 steps.

What are psychotropic medications?
Psychotropic medications are ‘any drug capable of affecting the mind, emotions and behaviour'
The three main classes of psychotropics prescribed are antidepressants, anxiolytic/hypnotics (mostly benzodiazepines to manage anxiety and insomnia) and antipsychotics. Other psychotropic classes include anticonvulsants and stimulants.

The Aged Care Quality and Safety Commission is helping providers to understand issues and their responsibilities around minimising the use of chemical and physical restraint. This includes ensuring that providers are appropriately documenting each instance of use.









